A surge in cases of dengue has been reported worldwide over the past few months. According to the data of the European Centre for Disease Control and Prevention, a total of over 12 million dengue cases and more than 8,000 dengue-related fatalities have been reported across 86 countries since the beginning of 2024. Among these countries, Brazil has reported the highest number of cases this year, exceeding 9 million followed by Argentina, Paraguay, Peru, and Colombia.
According to data published on the National Centre for Vector Borne Diseases Control’s website, India has reported 19,447 dengue cases and 16 fatalities as of April 30, 2024. The highest number of dengue cases reported was in 2023 with the WHO Region of the Americas reporting 4.5 million cases, with 2300 deaths. A high number of cases were reported in Asia: Bangladesh (321 000), Malaysia (111 400), Thailand (150 000), and Viet Nam (369 000).
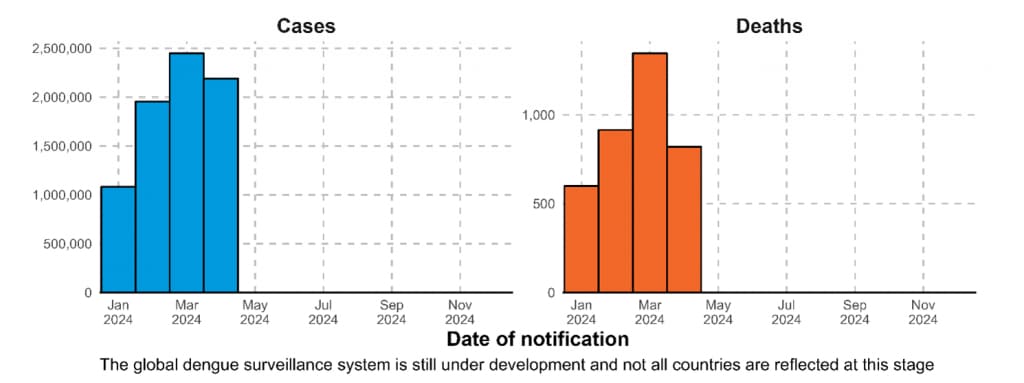
Figure 1. Epidemic curve of dengue cases and deaths as reported to WHO from January to April 2024*
Taking to the Firstpost about the current treatment protocol for dengue fever, Dr Tushar Tayal, Consultant, Internal Medicine, CK Birla Hospital (Gurugram) said that the primary focus of treating dengue fever is supportive care, which centers on managing fluids to prevent dehydration, particularly in severe cases such as dengue hemorrhagic fever or dengue shock syndrome.
“To alleviate pain and reduce fever, Paracetamol is employed. However, Non-Steroidal Anti-Inflammatory Drugs (NSAIDs) like aspirin or ibuprofen are not used, as they can increase the risk of bleeding. Continuous monitoring of vital signs and clinical parameters is essential to identify any progression towards severe dengue,” he added.
Key facts
*Dengue is a viral infection primarily transmitted through the bite of infected female Aedes aegypti mosquitoes. These mosquitoes typically bite during the day, with peak periods at dawn and dusk. It is more common in tropical and subtropical climates.
*Dengue is a viral infection transmitted to humans through the bite of infected mosquitoes.
*Dengue is found in tropical and sub-tropical climates worldwide, mostly in urban and semi-urban areas.
*While many dengue infections are asymptomatic or produce only mild illness, the virus can occasionally cause more severe cases and even death.
*Prevention and control of dengue depend on vector control. There is no specific treatment for dengue/severe dengue, and early detection and access to proper medical care greatly lower fatality rates of severe dengue.
The factors contributing to dengue’s spread include High population densities and poor sanitation creating breeding grounds for mosquitoes, said Dr Tushar, adding that warm, humid climates and rainy seasons support mosquito breeding.
Symptoms
*Most people with dengue have mild or no symptoms and will get better in 1–2 weeks. Rarely, dengue can be severe and lead to death. If symptoms occur, they usually begin 4–10 days after infection and last for 2–7 days. Symptoms may include high fever (40°C/104°F), severe headache, pain behind the eyes, muscle and joint pains, nausea, vomiting, swollen glands and rash.
*People who are infected for the second time are at greater risk of severe dengue.
Diagnostics and treatment
There is no specific treatment for dengue. The focus is on treating pain symptoms. Most cases of dengue fever can be treated at home with pain medicine. According to WHO, Acetaminophen (paracetamol) is often used to control pain. Non-steroidal anti-inflammatory drugs like ibuprofen and aspirin are avoided as they can increase the risk of bleeding.
Role of fluid management in treating dengue
Dr Tushar said that effective fluid management is a critical aspect of treating dengue, especially in severe cases. The primary objective is to prevent or manage dehydration and shock caused by plasma leakage, a common complication in severe dengue, he said, adding that in mild cases, oral rehydration is recommended, while intravenous fluids are administered in more severe cases or when oral intake is inadequate. He further said that the aim is to strike a balance in fluid administration to prevent dehydration and prevent the blood from becoming concentrated.
Importance of monitoring platelet count and other blood parameters
According to Dr Tushar, regular monitoring of blood parameters is crucial for patients diagnosed with Dengue. This includes frequent checks on:
Platelet count: Monitoring platelet levels helps assess the risk of bleeding, particularly if the count falls below 10,000, indicating a potential increase in bleeding risk.
Hematocrit levels: Hematocrit monitoring is essential to detect hemoconcentration, a sign of plasma leakage, which can lead to severe dengue.
Liver Function Test (LFT): LFT monitoring helps assess liver injury and potential liver failure, a rare but severe complication of Dengue.
In moderate Dengue cases, platelets and other parameters are typically checked daily. However, in severe cases, monitoring may be required every 12 hours, depending on the patient’s clinical condition, to ensure timely intervention and appropriate management.
Transmission through the mosquito bite
The dengue virus is transmitted to humans through the bites of infected female mosquitoes, primarily the Aedes aegypti mosquito. Other species within the Aedes genus can also act as vectors, but their contribution is normally secondary to Aedes aegypti. However, in 2023, a surge in local transmission of dengue by Aedes albopictus (tiger mosquito) has been seen in Europe.
Dietary guidelines and lifestyle precautions for patients
It is important to follow essential dietary guidelines and adopt lifestyle precautions for patients affected by dengue. Dr Tushar listed some of the recommendations including:
Hydration: Adequate hydration is vital, particularly for dengue patients, to prevent dehydration. Consuming water, oral rehydration solutions, and fresh juices is highly recommended.
Diet: A balanced and nutritious diet is essential to support recovery. Opt for easily digestible foods rich in vitamins, minerals, and protein, such as soup, boiled vegetables, porridge, and fruits. Avoid consuming fatty and spicy foods, as they can be challenging to digest and may exacerbate the illness.
Rest: Adequate rest is crucial to allow the immune system to recover. Patients should ensure they get sufficient rest to aid in their recovery process.
Medication: As previously mentioned, Non-Steroidal Anti-Inflammatory Drugs (NSAIDs) like aspirin and ibuprofen should be avoided due to the increased risk of bleeding.
Human-to-mosquito transmission
Mosquitoes can become infected by people who are viremic with the dengue virus. This can be someone who has a symptomatic dengue infection, someone who is yet to have a symptomatic infection (they are pre-symptomatic), and also someone who shows no signs of illness (they are asymptomatic).
Human-to-mosquito transmission can occur up to 2 days before someone shows symptoms of the illness, and up to 2 days after the fever has resolved.
The risk of mosquito infection is positively associated with high viremia and high fever in the patient; conversely, high levels of DENV-specific antibodies are associated with a decreased risk of mosquito infection. Most people are viremic for about 4–5 days, but viremia can last as long as 12 days.
Maternal transmission
The primary mode of transmission of the dengue virus between humans involves mosquito vectors. There is evidence, however, of the possibility of maternal transmission (from a pregnant mother to her baby). At the same time, vertical transmission rates appear low, with the risk of vertical transmission seemingly linked to the timing of the dengue infection during the pregnancy. When a mother does have a dengue infection when she is pregnant, babies may suffer from pre-term birth, low birth weight, and fetal distress.
Other transmission modes
Rare cases of transmission via blood products, organ donation and transfusions have been recorded. Similarly, transovarial transmission of the virus within mosquitoes have also been recorded.
Prevention
*The mosquitoes that spread dengue are active during the day.
*Lower the risk of getting dengue by protecting yourself from mosquito bites by using clothes that cover as much of your body as possible and mosquito nets if sleeping during the day.
*Preventing mosquitoes from accessing egg-laying habitats by environmental management and modification.
*Disposing of solid waste properly and removing artificial man-made habitats that can hold water.
*Covering, emptying and cleaning domestic water storage containers every week as it breeds in fresh water.
Severe dengue symptoms often come after the fever has gone away:
*Severe abdominal pain
*Persistent vomiting
*Rapid breathing
*Bleeding gums or nose
*Fatigue
*Restlessness
*Blood in vomit or stool
*Being very thirsty
*Pale and cold skin
*Feeling weak.
Global burden
The global incidence of dengue has experienced a dramatic surge in recent decades, with reported cases to the World Health Organization (WHO) increasing exponentially from 505,430 in 2000 to 5.2 million in 2019. Globally, dengue cases have risen significantly over the past five years, with a notable escalation in the Region of the Americas. As of the end of April 2024, the region has reported over 7 million cases, surpassing the previous annual high of 4.6 million cases in 2023.
However, due to the majority of cases being asymptomatic or mild and self-managed, the actual number of dengue cases remains underreported. Furthermore, many cases are misdiagnosed as other febrile illnesses, contributing to the underestimation of the true burden of the disease.
The year 2023 saw the highest recorded number of dengue cases, affecting over 80 countries across all WHO regions. The ongoing transmission, combined with an unexpected spike in cases, resulted in a historic high of over 6.5 million cases and more than 7,300 dengue-related deaths reported since the beginning of 2023.
Several factors have contributed to the increasing risk of spread of the dengue epidemic, including the changing distribution of vectors, such as Aedes aegypti and Aedes albopictus mosquitoes, particularly in previously unaffected countries. Also, the consequences of El Niño phenomena in 2023 and climate change, leading to rising temperatures and high rainfall and humidity, have also played a role.
Fragile health systems during the COVID-19 pandemic, as well as political and financial instabilities in countries facing complex humanitarian crises and high population movements, have further exacerbated the situation.
Dengue is now endemic in over 100 countries across the WHO Regions of Africa, the Americas, the Eastern Mediterranean, Southeast Asia, and the Western Pacific. The Americas, Southeast Asia, and Western Pacific regions are the most severely affected, with Asia accounting for approximately 70% of the global disease burden. Moreover, dengue is spreading to new areas in Europe, the Eastern Mediterranean, and South America.
Source- With inputs from WHO.
Link to article –
Over 12 million cases, 8,000 deaths in 2024: Is dengue the new global pandemic?